Index
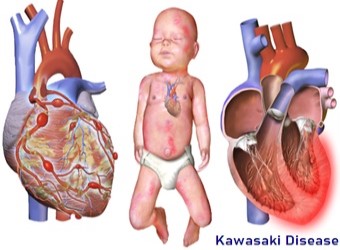
Kawasaki Disease
What Is Kawasaki Disease?
Kawasaki disease is a syndrome of unknown cause that results in a fever and mainly affects children under 5 years of age.
It is a form of vasculitis, where blood vessels become inflamed throughout the body.
The fever typically lasts for more than five days and is not affected by usual medications.
What Causes Kawasaki Disease?
The specific cause of Kawasaki disease is unknown. One possible explanation is that it may be due to an infection
triggering an autoimmune response in children who are genetically predisposed. The pathogenesis is complex and incompletely understood.
They believe it does not spread from person to person. It is most common among children of Japanese and Korean descent but can affect any child..

What are the Signs & Symptoms of Kawasaki Disease?
- GIT
Diarrhea, chest pain, abdominal pain, vomiting, liver dysfunction, pancreatitis, hydrops gallbladder,
parotitis,cholangitis, intussusception, intestinal pseudo-obstruction, ascites, splenic infarction.
- MSS Polyarthritis and arthralgia.
- CVS Myocarditis, pericarditis, tachycardia, valvular heart disease.
- GU Urethritis, prostatitis, cystitis, priapism, interstitial nephritis, orchitis, nephrotic syndrome.
- CNS Lethargy, semi coma, aseptic meningitis, and sensorineural deafness.
- RS Shortness of breath, influenza-like illness, pleural effusion, atelectasis.
- Skin Erythema and induration at BCG vaccination site, Beau's lines, and finger gangrene.
- MSS Polyarthritis and arthralgia.
- CVS Myocarditis, pericarditis, tachycardia, valvular heart disease.
- GU Urethritis, prostatitis, cystitis, priapism, interstitial nephritis, orchitis, nephrotic syndrome.
- CNS Lethargy, semi coma, aseptic meningitis, and sensorineural deafness.
- RS Shortness of breath, influenza-like illness, pleural effusion, atelectasis.
- Skin Erythema and induration at BCG vaccination site, Beau's lines, and finger gangrene.
HEART CONDITIONS Diseases and Treated FAQ's
Kawasaki disease can be diagnosed only clinically (i.e., by medical signs and symptoms). No specific laboratory test exists for this condition. Establishing the diagnosis is difficult, especially early in the course of the illness, and frequently children are not diagnosed until they have seen several health-care providers. Many other serious illnesses can cause similar symptoms, and must be considered in the differential diagnosis, including scarlet fever, toxic shock syndrome, juvenile idiopathic arthritis, and childhood mercury poisoning (infantile acrodynia).
Classically, five days of fever plus four of five diagnostic criteria must be met to establish the diagnosis.
Other typical diagnosis are:
- Erythema of the lips or oral cavity or cracking of the lips,
- Rash on the trunk,
- Swelling or erythema of the hands or feet,
- Red eyes (conjunctival injection),
- Swollen lymph node in the neck of at least 15 mm.
- Erythema of the lips or oral cavity or cracking of the lips,
- Rash on the trunk,
- Swelling or erythema of the hands or feet,
- Red eyes (conjunctival injection),
- Swollen lymph node in the neck of at least 15 mm.
Children with Kawasaki disease should be hospitalized and cared for by a physician who has experience with this disease.
When in an academic medical center, care is often shared between pediatric cardiology, pediatric rheumatology, and pediatric infectious
disease specialists (although no specific infectious agent has yet been identified). To prevent damage to the coronary arteries,
treatment should be started as soon as the diagnosis is made.
- Intravenous immunoglobulin (IVIG) is the standard treatment for Kawasaki disease and is administered in high doses with marked improvement usually noted within 24 hours. If the fever does not respond, an additional dose may have to be considered. In rare cases, a third dose may be given to the child. IVIG by itself is most useful within the first seven days of onset of fever, in terms of preventing coronary artery aneurysm. IVIG given within the first 10 days of the disease reduces the risk of damage to the coronary arteries in children, without serious adverse effects.
- Other treatments are available.
- Intravenous immunoglobulin (IVIG) is the standard treatment for Kawasaki disease and is administered in high doses with marked improvement usually noted within 24 hours. If the fever does not respond, an additional dose may have to be considered. In rare cases, a third dose may be given to the child. IVIG by itself is most useful within the first seven days of onset of fever, in terms of preventing coronary artery aneurysm. IVIG given within the first 10 days of the disease reduces the risk of damage to the coronary arteries in children, without serious adverse effects.
- Other treatments are available.
With early treatment, rapid recovery from the acute symptoms can be expected, and the risk of coronary artery aneurysms
is greatly reduced. Untreated, the acute symptoms of Kawasaki disease are self-limited (i.e. the patient will recover eventually),
but the risk of coronary artery involvement is much greater, even many years later. Many cases of myocardial infarction in young adults
have now been attributed to Kawasaki disease that went undiagnosed during childhood. Overall, about 2% of patients die from complications of coronary vasculitis.
Laboratory evidence of increased inflammation combined with demographic features (male sex, age less than six months or greater than eight years) and incomplete response to IVIG therapy create a profile of a high-risk patient with Kawasaki disease. The likelihood that an aneurysm will resolve appears to be determined in large measure by its initial size, in which the smaller aneurysms have a greater likelihood of regression. Other factors are positively associated with the regression of aneurysms, including being younger than a year old at the onset of Kawasaki disease, fusiform rather than saccular aneurysm morphology, and an aneurysm location in a distal coronary segment. The highest rate of progression to stenosis occurs among those who develop large aneurysms. The worst prognosis occurs in children with giant aneurysms.[135] This severe outcome may require further treatment such as percutaneous transluminal angioplasty, coronary artery stenting, bypass grafting, and even cardiac transplantation.
A relapse of symptoms may occur soon after initial treatment with IVIG. This usually requires rehospitalization and retreatment. Treatment with IVIG can cause allergic and nonallergic acute reactions, aseptic meningitis, fluid overload, and rarely, other serious reactions. Overall, life-threatening complications resulting from therapy for Kawasaki disease are exceedingly rare, especially compared with the risk of nontreatment. Evidence indicates Kawasaki disease produces altered lipid metabolism that persists beyond the clinical resolution of the disease.
Laboratory evidence of increased inflammation combined with demographic features (male sex, age less than six months or greater than eight years) and incomplete response to IVIG therapy create a profile of a high-risk patient with Kawasaki disease. The likelihood that an aneurysm will resolve appears to be determined in large measure by its initial size, in which the smaller aneurysms have a greater likelihood of regression. Other factors are positively associated with the regression of aneurysms, including being younger than a year old at the onset of Kawasaki disease, fusiform rather than saccular aneurysm morphology, and an aneurysm location in a distal coronary segment. The highest rate of progression to stenosis occurs among those who develop large aneurysms. The worst prognosis occurs in children with giant aneurysms.[135] This severe outcome may require further treatment such as percutaneous transluminal angioplasty, coronary artery stenting, bypass grafting, and even cardiac transplantation.
A relapse of symptoms may occur soon after initial treatment with IVIG. This usually requires rehospitalization and retreatment. Treatment with IVIG can cause allergic and nonallergic acute reactions, aseptic meningitis, fluid overload, and rarely, other serious reactions. Overall, life-threatening complications resulting from therapy for Kawasaki disease are exceedingly rare, especially compared with the risk of nontreatment. Evidence indicates Kawasaki disease produces altered lipid metabolism that persists beyond the clinical resolution of the disease.