Index
Coarctation of Aorta
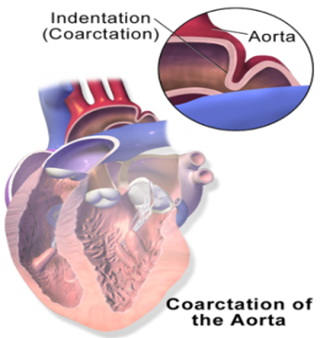
What Is Coarctation of the Aorta?
Also called aortic narrowing, is a congenital condition whereby the aorta is narrow, usually in the area where the ductus arteriosus (ligamentum arteriosum after regression) inserts.
The word coarctation means "pressing or drawing together; narrowing". Coarctations are most common in the aortic arch. The arch may be small in babies with coarctations.
Other heart defects may also occur when coarctation is present, typically occurring on the left side of the heart.
What Causes Coarctation of the Aorta?
There are three types of Aortic Coarctations:- Preductal Coarctation
The narrowing is proximal to the ductus arteriosus. Blood flow to the aorta that is distal to the narrowing is dependent on the ductus arteriosus;
therefore severe coarctation can be life-threatening. Preductal coarctation results when an intracardiac anomaly during fetal life decreases blood flow through the left side of the heart,
leading to hypoplastic development of the aorta. This is the type seen in approximately 5% of infants with Turner syndrome.
- Ductal CoarctationThe narrowing occurs at the insertion of the ductus arteriosus. This kind usually appears when the ductus arteriosus closes.
- Postductal CoarctationThe narrowing is distal to the insertion of the ductus arteriosus. Even with an open ductus arteriosus, blood flow to the lower body can be impaired.
This type is most common in adults. It is associated with notching of the ribs (because of collateral circulation), hypertension in the upper extremities, and weak pulses in the lower extremities.
Postductal coarctation is most likely the result of the extension of a muscular artery (ductus arteriosus) into an elastic artery (aorta) during fetal life,
where the contraction and fibrosis of the ductus arteriosus upon birth subsequently narrows the aortic lumen.

What are the Signs & Symptoms of Coarctation of the Aorta?
In mild cases, children may show no signs or symptoms at first and their condition may not be diagnosed until later in life.
Some children born with coarctation of the aorta have additional heart defects, such as aortic stenosis, ventricular septal defect, patent ductus arteriosus or mitral valve abnormalities.
Coarctation is about twice as common in boys as it is in girls. It is common in girls who have Turner syndrome.
Symptoms may be absent with mild narrowings (coarctation). When present, they include breathing difficulties, poor appetite or trouble feeding, and failure to thrive.
Later on, children may develop symptoms related to problems with blood flow and an enlarged heart.
They may experience dizziness or shortness of breath, fainting or near-fainting episodes, chest pain, abnormal tiredness or fatigue, headaches, or nosebleeds. They have cold legs and feet or have pain in their legs with exercise (intermittent claudication).
Some children born with coarctation of the aorta have additional heart defects, such as aortic stenosis, ventricular septal defect, patent ductus arteriosus or mitral valve abnormalities.
Coarctation is about twice as common in boys as it is in girls. It is common in girls who have Turner syndrome.
Symptoms may be absent with mild narrowings (coarctation). When present, they include breathing difficulties, poor appetite or trouble feeding, and failure to thrive.
Later on, children may develop symptoms related to problems with blood flow and an enlarged heart.
They may experience dizziness or shortness of breath, fainting or near-fainting episodes, chest pain, abnormal tiredness or fatigue, headaches, or nosebleeds. They have cold legs and feet or have pain in their legs with exercise (intermittent claudication).
HEART CONDITIONS Diseases and Treated FAQ's
With imaging, resorption of the lower part of the ribs may be seen,
due to increased blood flow over the neurovascular bundle that runs there.
Prestenotic dilatation of the aortic arch and left subclavian artery, as well as indentation at the site of coarctation results in a classic 'figure 3 sign' on x-ray.
The characteristic bulging of the sign is caused by dilatation of the aorta due to an indrawing of the aortic wall at the site of cervical rib obstruction, with consequent poststenotic dilatation.
This physiology results in the '3' image for which the sign is named.
When the esophagus is filled with barium, a reverse 3 or E sign is often seen and represents a mirror image of the areas of prestenotic and poststenotic dilatation.
Prestenotic dilatation of the aortic arch and left subclavian artery, as well as indentation at the site of coarctation results in a classic 'figure 3 sign' on x-ray.
The characteristic bulging of the sign is caused by dilatation of the aorta due to an indrawing of the aortic wall at the site of cervical rib obstruction, with consequent poststenotic dilatation.
This physiology results in the '3' image for which the sign is named.
When the esophagus is filled with barium, a reverse 3 or E sign is often seen and represents a mirror image of the areas of prestenotic and poststenotic dilatation.
The first operations to treat coarctation were carried out by Clarence Crafoord in Sweden in 1944.
Some patients found to have coarctation, treatment is conservative if asymptomatic, but may require surgical resection of the narrow segment if there is arterial hypertension.
Treatment options for coarctation of the aorta depend on your age at the time of diagnosis and the severity of your condition.
Other heart defects might be repaired at the same time as aortic coarctation. Treatment approaches usually consist of surgery or a procedure called balloon angioplasty or stent placement. In some cases angioplasty can be performed to dilate the narrowed artery, with or without the placement of a stent graft.
Some patients found to have coarctation, treatment is conservative if asymptomatic, but may require surgical resection of the narrow segment if there is arterial hypertension.
Treatment options for coarctation of the aorta depend on your age at the time of diagnosis and the severity of your condition.
Other heart defects might be repaired at the same time as aortic coarctation. Treatment approaches usually consist of surgery or a procedure called balloon angioplasty or stent placement. In some cases angioplasty can be performed to dilate the narrowed artery, with or without the placement of a stent graft.
Risk factors Coarctation of the aorta often occurs along with other congenital heart defects,
although doctors don't know what causes multiple heart defects to form together. The condition is more common in males than in females.
You or your child may be more likely to have aortic coarctation if certain heart conditions exist, including:
- Bicuspid Aortic Valve
The aortic valve separates the lower left chamber (left ventricle) of the heart from the aorta. A bicuspid aortic valve has two flaps (cusps) instead of the usual three. Many people with coarctation of the aorta have a bicuspid aortic valve.
- Patent Ductus Arteriosus
Before birth, the ductus arteriosus is a blood vessel connecting the left pulmonary artery to the aorta — allowing blood to bypass the after birth, the ductus arteriosus usually closes. If it remains open, it's called a patent ductus arteriosus.
- Holes in the Wall (Between the left and right sides of the heart.)
You may have a hole in the wall (septum) between the upper chambers of the heart (atrial septal defect) or the lower chambers of the heart (ventricular septal defect) when you're born. This causes oxygen-rich blood from the left side of the heart to mix with oxygen-poor blood in the right side of the heart.
- Aortic Valve Stenosis
This is a narrowing of the valve that separates the left ventricle of the heart from the aorta (aortic valve). This means your heart has to pump harder to get adequate blood flow to your body. Over time, this can cause your heart muscle to thicken and lead to symptoms such as chest pain, fainting spells and breathlessness, or heart failure.
- Aortic Valve Regurgitation
This occurs when the aortic valve doesn't close tightly, causing blood to leak backward into the left ventricle.
- Mitral Valve Stenosis
This is a narrowing of the valve (mitral valve) between the upper left heart chamber (left atrium) and the left ventricle that lets blood flow through the left side of your heart. In this condition, blood may back up into your lungs, causing shortness of breath or lung congestion. Like aortic valve stenosis, this condition can also lead to heart failure.
- Mitral valve regurgitation
This occurs when the mitral valve doesn't close tightly, causing blood to leak backward into the left atrium.
- Bicuspid Aortic Valve
The aortic valve separates the lower left chamber (left ventricle) of the heart from the aorta. A bicuspid aortic valve has two flaps (cusps) instead of the usual three. Many people with coarctation of the aorta have a bicuspid aortic valve.
- Patent Ductus Arteriosus
Before birth, the ductus arteriosus is a blood vessel connecting the left pulmonary artery to the aorta — allowing blood to bypass the after birth, the ductus arteriosus usually closes. If it remains open, it's called a patent ductus arteriosus.
- Holes in the Wall (Between the left and right sides of the heart.)
You may have a hole in the wall (septum) between the upper chambers of the heart (atrial septal defect) or the lower chambers of the heart (ventricular septal defect) when you're born. This causes oxygen-rich blood from the left side of the heart to mix with oxygen-poor blood in the right side of the heart.
- Aortic Valve Stenosis
This is a narrowing of the valve that separates the left ventricle of the heart from the aorta (aortic valve). This means your heart has to pump harder to get adequate blood flow to your body. Over time, this can cause your heart muscle to thicken and lead to symptoms such as chest pain, fainting spells and breathlessness, or heart failure.
- Aortic Valve Regurgitation
This occurs when the aortic valve doesn't close tightly, causing blood to leak backward into the left ventricle.
- Mitral Valve Stenosis
This is a narrowing of the valve (mitral valve) between the upper left heart chamber (left atrium) and the left ventricle that lets blood flow through the left side of your heart. In this condition, blood may back up into your lungs, causing shortness of breath or lung congestion. Like aortic valve stenosis, this condition can also lead to heart failure.
- Mitral valve regurgitation
This occurs when the mitral valve doesn't close tightly, causing blood to leak backward into the left atrium.